The opinions expressed in this article are those of Dr. Charles Mackay and for general information purposes only.
Despite its prevalence in Canada, there’s still plenty of misunderstanding surrounding addiction and substance use disorder.
According to the Centre for Addiction and Mental Health, “one in seven Canadians aged 15 or older (about 3.5 million people) have problems with alcohol; one in 20 (about 1.5 million people) have problems with cannabis…”
Addiction education helps prevent unsafe drug use and reduces stigma, which can create significant barriers for people who use drugs when it comes to accessing life saving services.
We talked with Dr. Mackay, a ASAM (American Society of Addiction Medicine) and ABAM (American Board of Addiction Medicine) certified general practitioner. Dr. Mackay, who is a clinician at Edgewood Health Network’s Nouveau Depart clinic in Quebec, has 30 years experience in the field of addiction.
What is addiction?
Addiction is a term used to describe both substance use disorder or loss of control when it comes to a substance or a behaviour. It’s much more complex than really enjoying a substance or activity: we often hear people say they’re “addicted” to coffee or talk about “binging” a TV show.
But when a person is addicted to a substance (like alcohol or drugs), they fall into a harmful pattern of consumption despite negative outcomes and a desire to stop. There are often symptoms of dependence, including an increased tolerance and withdrawal symptoms. Addiction can impact every aspect of a person’s life.
Clinicians often use the four C’s to describe addiction: Craving, loss of control, compulsion to use and use despite consequences.
Let’s consider an example of someone who is likely experiencing an addiction: Emma is a 50-year-old mother of two with a high-stress job. She starts having one or two glasses of wine in the evenings to end a stressful work day. As time progresses, she is having at least five drinks a night and waking up hungover. Her work performance starts to slip and her boss tells her she needs to improve or she could lose her job.
Is addiction a disease?
Yes, addiction has been classified as a disease for at least 200 years. Swedish physician Dr. Magnus Huss was the first to use the term addiction in his 1849 essay “Alcoholismus Chronicus.” Clinicians helped reduce stigma when they stopped viewing addiction as a “choice.” Stigmatizing and criminalizing drug and substance use has created significant barriers to treatment and harm reduction services.
In 1956, the American Medical Association declared alcoholism a disease, which accelerated the development of treatments and reduced stigma around the condition. As a result, individuals with alcohol use disorders were less afraid of judgement and therefore more likely to seek help.
The American Psychiatric Association and the World Health Organization also agree that addiction is, by definition, a chronic disease. Like other chronic illnesses, symptoms affect people over an extended period of time and evolve slowly.
How do psychoactive substances affect the brain?
In short, psychoactive substances are chemicals or drugs that affect the mental state or brain function in some way. These include cannabis, cocaine, alcohol or even prescription medications like painkillers.
There are several models and theories about how these drugs affect our brains, and the creation of neuroimaging technology has helped clinicians paint a clearer picture of how and where addiction acts.
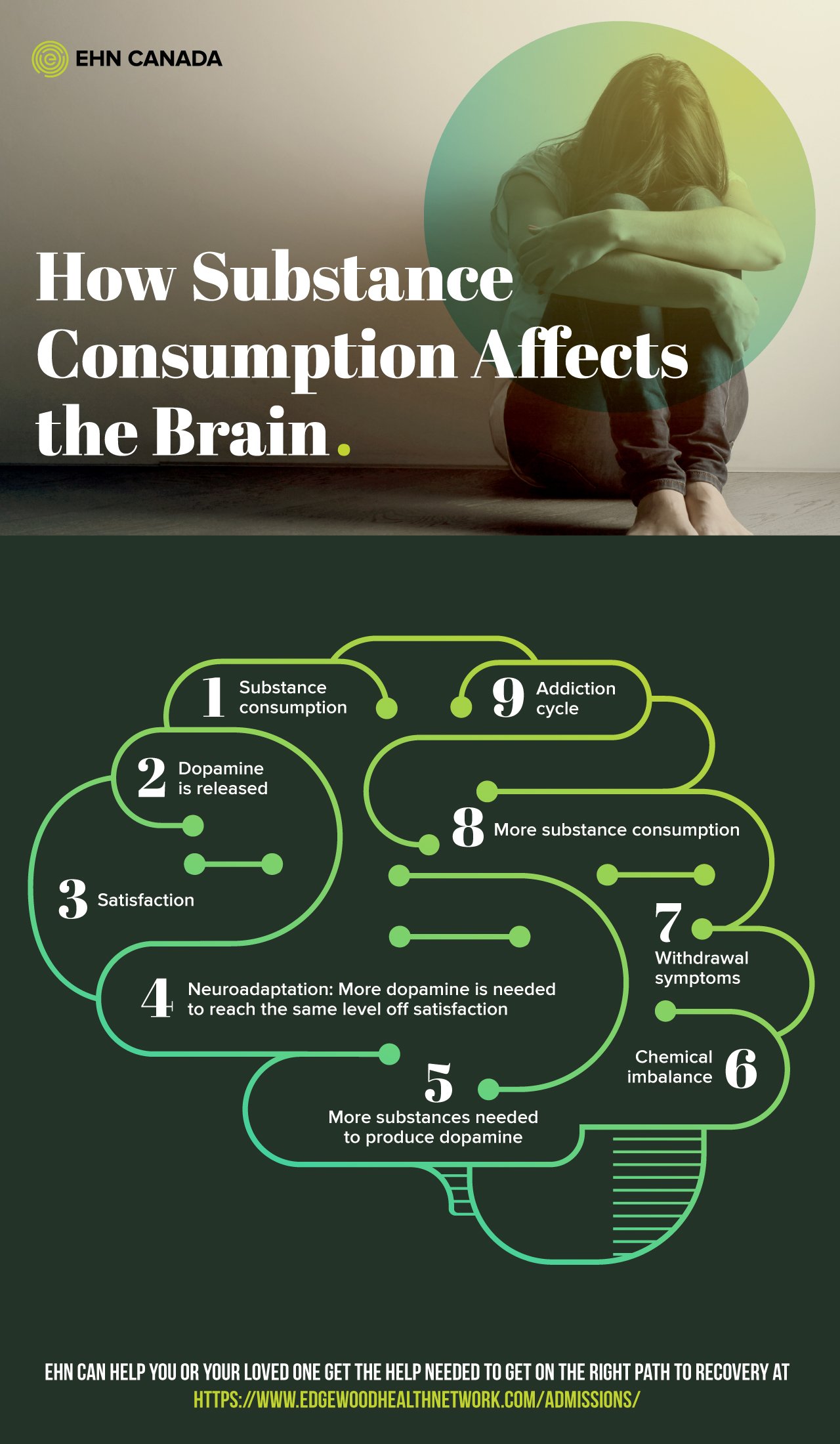
When we consume a drug, the reward centre of our brain releases a neurochemical called dopamine and creates feelings of satisfaction or happiness. Dopamine plays an important role in movement, motivation and behaviour reinforcement, so substance use has a direct impact on the brain and quietly changes our actions and reactions. Over time, neuroadaptation occurs: our brains adapt and a higher level of dopamine (so, a higher dose of our drug of choice) is needed to create the same satisfying or happy feelings.
Do psychoactive substances affect the brain permanently?
The effects of neuroadaptation don’t resolve quickly, even after someone stops using the substance that caused it. Because these changes can take a long time to resolve, people in recovery are vulnerable to relapse. However, each person is different. Think about how some people can kick a smoking habit by going cold turkey, while others take several failed attempts to quit before it sticks.
Early identification and treatment of addiction or harmful drug use can limit the changes to the brain and make recovery more likely.
Why do some people become addicted while others don’t?
We know that many people can experiment with alcohol, drugs, or certain behaviours without becoming addicted. Why do only some people develop a dependence?
Addiction is a complex issue and there are several different models used to understand it, but it is widely accepted that a combination of biological and social factors are usually at play. We know that there is not one single factor that will reliably predict that some one will develop a substance use disorder or addiction.
Genetics, social environments and/or social exclusion, concurrent mental illness, and past trauma, are just some risk factors for substance use problems.
It is important to look at the social determinants of health when we consider how certain people become addicted while others do not.
How do genetics play a role in addiction?
We know that genetics can play a role in the development of addiction, but this doesn’t mean every person a history of addiction or alcohol use disorder in their family will develop substance use issues.
According to the Society for Clinical Pharmacology and Therapeutics, “addictions are moderately to highly heritable. Family, adoption, and twin studies reveal that an individual’s risk tends to be proportional to the degree of genetic relationship to an addicted relative.” In simper terms, the more genetically similar somebody is to a relative who struggles with addiction, the more likely they are to develop an addiction themselves.
Several academic studies explore the genetic component of substance use disorders. For example, the controversial twin/triplet studies of the 1960s found that genetics is one of the determining factors for alcohol dependence. Similarly, a 2014 Cambridge University study confirmed that heredity is about 50% responsible for a substance use disorder, but that the social environment (including early relationships, education, social inclusion or exclusion) also has a significant impact.
Are there different “types” of substance use problems?
Clinicians have been trying to classify addiction since the 19th century. It’s a difficult task, as a cause isn’t as clear as other with types of disease, such as diabetes. Whereas diabetics can be diagnosed with Type 1 or Type 2, it is not so simple to categorize addiction. But, effective treatment cannot be started until a diagnosis is made.
Elvin Morton Jellinek, a biotstatistician, psychologist and researcher of alcohol-related disorders, was first to classify alcoholism scientifically. He developed a comprehensive, evidence-based theory that confirmed alcoholism is indeed a disease. In the mid-20th century, Jellinek conducted a clinical study of people with chronic alcoholism, where he sought to establish how the disease develops over time. It was from this study that he eventually created the Jellinek Curve. This U-shaped curve shows the progression or phases of the disease, step-by-step.
Methods of categorizing addiction have evolved since then, but Jellinek’s work led to a better understanding of addiction in order to find more effective treatment and care. Today, specialists use the model presented in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The DSM is used by healthcare professionals as a guidebook to diagnose mental illnesses.
How should I talk to youth about substance use?
When it comes to talking to your kids or other young people about substance use, it’s important to be honest. It’s possible to talk about the risks and consequences of addiction without dealing in myths like, “you will become addicted the first time you try a drug.” A young person who is educated and aware will be able to make better, safer choices.
Prevention is most effective when truthful, factual information is used. You don’t have to terrify your kids with anecdotes about drug use; this can often have the opposite effect if the young person no longer trusts you as a reliable source of information.
At any age, we make smart decisions when we’re well informed of the risks and consequences of our choices. When it comes to substances, knowing the facts helps us to make better choices early on in life to prevent the development of addiction or unsafe use.
How is addiction treated?
The first step in treatment is typically detoxification and an assessment for any concurrent, or co-occuring, mental health disorders. In the case of co-occurring disorders, integrated treatment plans are best to help address both issues at once. A holistic treatment model helps prevent relapse by reducing the chance that the substance use will affect the mental health problem or vice versa. Some people will require medicine and supervision to tolerate withdrawal symptoms, such as fever and body aches.
Someone who is opioid-dependant might choose to start maintenance therapy, where they’ll take an oral dose of medication, like methadone, under medical supervision. This helps reduce cravings and reduce symptoms of withdrawal.
To date, there are only a few pharmacological approaches with a modest therapeutic response for alcohol use disorders.
Other non-medical options for treating addiction include inpatient or outpatient therapy and support groups. Evidence-based therapies help individuals regain control over their substance use and achieve sobriety. One example of this is Cognitive Behavioural Therapy (CBT), which is designed to help control harmful, negative thought patterns.
There is no one-size-fits all solution and several approaches and goals of treatment are possible. A treatment plan must be personalized, therefore, it is important that any person in treatment is involved in determining their plan with the guidance of a registered professional or treatment facility
Where can I seek help for an addiction?
You do a fair amount of research before choosing a course of treatment for yourself or a loved one. When reaching out to a facility or treatment centre, here are some important questions to ask:
- Is there an initial medical assessment to provide you with a personalized treatment plan?
- Are there subsequent assessments throughout treatment to ensure that it continues to meet your needs?
- Is there medical supervision?
- Are the therapists accredited and registered with a professional college, like the College of Psychologists of Ontario?
- Does the treatment include aftercare?
- Is there a family support program?
Remember that there is no one-size-fits-all solution or treatment program, and that you deserve qualified, empathetic treatment that is tailored to your unique situation.
ABOUT EHN CANADA
EHN Canada is the nation’s largest network of industry-leading mental health, trauma, and addiction treatment facilities, each with a passion for providing quality treatment for Canadians. We are committed to both caring for our patients and supporting their loved ones. With over 75 years of collective experience, our inpatient, outpatient, and online programs are offered across the country, providing essential compassionate care to patients wherever they are.
To learn more, please visit www.ehncanada.com.
References
“Alcoholism.” n.d. In Encyclopædia Britannica.
Babor, Thomas F. 1996. “The Classification of Alcoholics: Typology Theories from the 19th Century to the Present.” Alcohol Health and Research World 20 (1): 6–14.
Canada, Santé. 2018. “Stigmatisation Entourant La Consommation de Substances.” Canada.ca. 19 février 2018. https://www.canada.ca/fr/sante-canada/services/dependance-aux-drogues/consommation-problematique-medicaments-ordonnance/opioides/stigmatisation.html.
“How Long Has Addiction Been Classified as A Disease?” 2019. Vertavahealth.Com. 3 octobre 2019. https://vertavahealth.com/blog/how-long-addiction-classified-disease/.
Jellinek, E. M. (1942) Alcohol Addiction and Chronic Alcoholism. Yale University Press, New Haven.
Jellinek, E. M. (1960) The Disease Concept of Alcoholism. Hillhouse, New Brunswick.
Kathy Bettinardi-Angres, MS, RN, APN, CADC, and Daniel H. Angres. n.d. “Understanding the Disease of Addiction.”
Miller, Peter M., ed. 2014. Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. P. 72. Academic Press.
National Institute on Drug Abuse. 2018. “Understanding Drug Use and Addiction DrugFacts.” Drugabuse.Gov. 6 juin 2018. https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction.
“OMS | Maladies Chroniques.” 2014. https://www.who.int/topics/chronic_diseases/fr/.
Verhulst, B., M. C. Neale, and K. S. Kendler. 2015. “The Heritability of Alcohol Use Disorders: A Meta-Analysis of Twin and Adoption Studies.” Psychological Medicine 45 (5): 1061–72.