When a mental health disorder causes a substance abuse problem, the condition is called a co-occurring or concurrent disorder (also known as or dual-diagnosis or comorbidity). Simply put, it means having both an addiction and a mental health disorder at the same time or at different times.
When mental health disorders are left untreated, they cause relapses, making rehabilitation from substance abuse much harder to achieve.
Statistics Canada data from 2012 estimated that 282,000 Canadians (1.2% of the population) aged 15 to 64 had experienced a combination of a mood or anxiety disorder and an alcohol or drug use disorder within the past year. [1]
Mental health disorder is a disease that needs to be treated
Mental illness is defined as a change or “a disturbance in your thought, perceptions and emotions that affects your ability to think, make decisions and function on a day-to-day basis. There are degrees of mental illness. It can vary from mild to severe. However, any version merits diagnosis and treatment”. [2]
Mental health disorders can happen like a cold or any other disease. Rather than a weakness, mental illness is a biological condition that is triggered by the social environment.
If you have high blood sugar, you would see a specialist. If you broke your arm, you would get an X-ray and a cast from a doctor. It’s just as important to seek treatment for a chronic mental health disorder from a medical professional.
Why underlying mental conditions can cause addictions
Both substance use and mental health disorders affect the same part of the brain, so it’s unsurprising that addictions and mental health disorders are often concurrent. [3] Some studies suggest that concurrent disorders may happen for one of two reasons. [4]
First, a person’s underlying genetic and environmental factors could be evenly increasing the risk of both the substance abuse and mental health disorder (we’ll talk more about genetic and environmental factors below).
Second, the two disorders could have inter-related effects: as one disorder worsens, the risk of developing the other increases. For example, someone suffering from a mental health disorder, like anxiety or depression, just wants to get better. Substances provide temporary relief from overwhelming situations. They might seem like the perfect solution at first, but they only worsen the situation. Over time, tolerance builds and greater quantities of the substance are needed to achieve the same sense of well-being, leading to an addiction.
Can substance abuse cause mental illness?
Yes, an addiction problem can also create a mental disorder over time. Psychoactive substances change the structure and neurochemistry of the brain. For example, long-term use of cannabis that began in youth can lead to psychosis or hallucinations in adulthood. Continued use of cocaine can create depression because it over-stimulates the body and mind. When use stops, it can take up to five years to recover from the mental disorder.
I have a good job, a healthy family—it can’t be happening to me
Substance abuse and mental health disorders can happen to anyone with a predisposition who experiences a trauma. It is a question of genetics and social environment.
“I treated lawyers that couldn’t deal with the work overload; stressed teachers who were having too much to drink every evening; doctors, newly retired people who were bored and felt useless; persons from all social and economic backgrounds. It’s a chronic mental health disorder, it’s a disease, and it can happen to everyone with a predisposition, like every other type of disease.”
Lucy Di Santo, counsellor at EHN Bellwood Toronto
Can COVID-19 be a traumatic event?
According to the American Psychological Association, “trauma refers to events or experiences that are shocking and overwhelming, typically involving major threats to the physical, emotional, or psychological safety and well-being of the individual victim(s) and loved ones and friends (as well as to others). Its original occurrence is usually sudden and unexpected and it may be a one-time event”. [5]
COVID-19 falls in that category.
The pandemic has created a climate of uncertainty and fear that affects many areas of life, such as health, work, finances, and family. Individuals have no control over the current situation, and this loss of control often creates worry. While staying home and adopting new habits are important for public health measures, they have also become daily reminders of the uncertainty that surrounds us.
A poll found that 50% of Canadians reported worsening mental health since COVID-19, specifically with many feeling worried or anxious. [6]
The Canadian Centre on Substance Use and Addiction agrees that substance use in Canada is also on the rise during the pandemic. A recent poll found that, since physical distancing and self-isolation began, 25% of Canadians aged 35-54 and 21% of those aged 18-34 have increased their alcohol consumption. [7]
Why is the concurrent disorder surfacing now?
“When a major event happens, people with this biological component are more likely to turn to drugs or alcohol to cope, and develop an addiction over time. If that trauma were never to happen, the substance abuse might have never started. It would be dormant,” explains Lucy.
Furthermore, everyone’s response to trauma is unique. The American Psychological Association reports that “individuals’ post-trauma reactions show great variability, ranging from those that are highly resilient–with little or no emotional distress– to those that are relatively mild and short-term, to those that are major, chronic, and highly debilitating. Disorders of medical or mental health may or may not follow”. [8]
While many people are experiencing collective trauma from COVID-19 related events, life is still happening all around us–unfortunately, people are experiencing many other kinds of trauma as well. “Epidemiological research has demonstrated that traumatic events are common and thus most humans will experience a potentially traumatic event at some point in their lifetime.” [9]
Genetic vulnerabilities
The National Institute on Drug Abuse estimates “40–60% of an individual’s vulnerability to substance use disorders is attributable to genetics”. Some people may be more vulnerable to a substance abuse or mental health disorder based on complex genetic interactions with environmental influences. In their example, the National Institute on Drug Abuse notes that “frequent marijuana use during adolescence is associated with increased risk of psychosis in adulthood, specifically among individuals who carry a particular gene variant”. [10]
However, sometimes one’s genes can specifically predispose them towards a dependence. For example, a protein can influence how a person responds to a drug, determining if the experience feels good or not, or how long a drug remains in one’s body. [11] Someone whose genes allow them to enjoy a substance experience has a biological obstacle that may not exist for someone who feels terrible from the substance experience.
Environmental influences
Many situations can increase the risk of having a mental disorder or substance abuse problem surfacing. Environmental factors like stress, bad childhood experience or trauma, can trigger one of the disorders.
Knowing something is off is a step in the right direction
“There are some stages before recognizing there’s a problem,” says Lucy. “The person doesn’t know first-hand that something is not right.”
1. First stage: no awareness. Staying in all day, every day, and having more than one drink while watching TV doesn’t seem like a problem. Then something happens. It could be a DUI, or falling asleep and missing an important appointment.
2. Second stage: knowing there’s a problem. Most of the time, people won’t get help right away. Why? It’s mostly a cultural problem: the fear of judgement, feeling ashamed. They believe they can do it on their own (and society tells them the same). Instead, they find a substance along the way to make them feel better, and their tolerance builds up the more they drink or use.
This is called self-medication. And it’s not the key to recovering. It presents high risks in any situation, but even more in the case of a co-occurring disorder.
Dangers of self-medicating with a co-occurring disorder include:
- Hiding the signs of mental health disorder
- Developing a long-term addiction
- Exacerbating the symptoms of mental illness
- Fostering isolation, instead of connection, from others
- Not getting treatment for the underlying condition
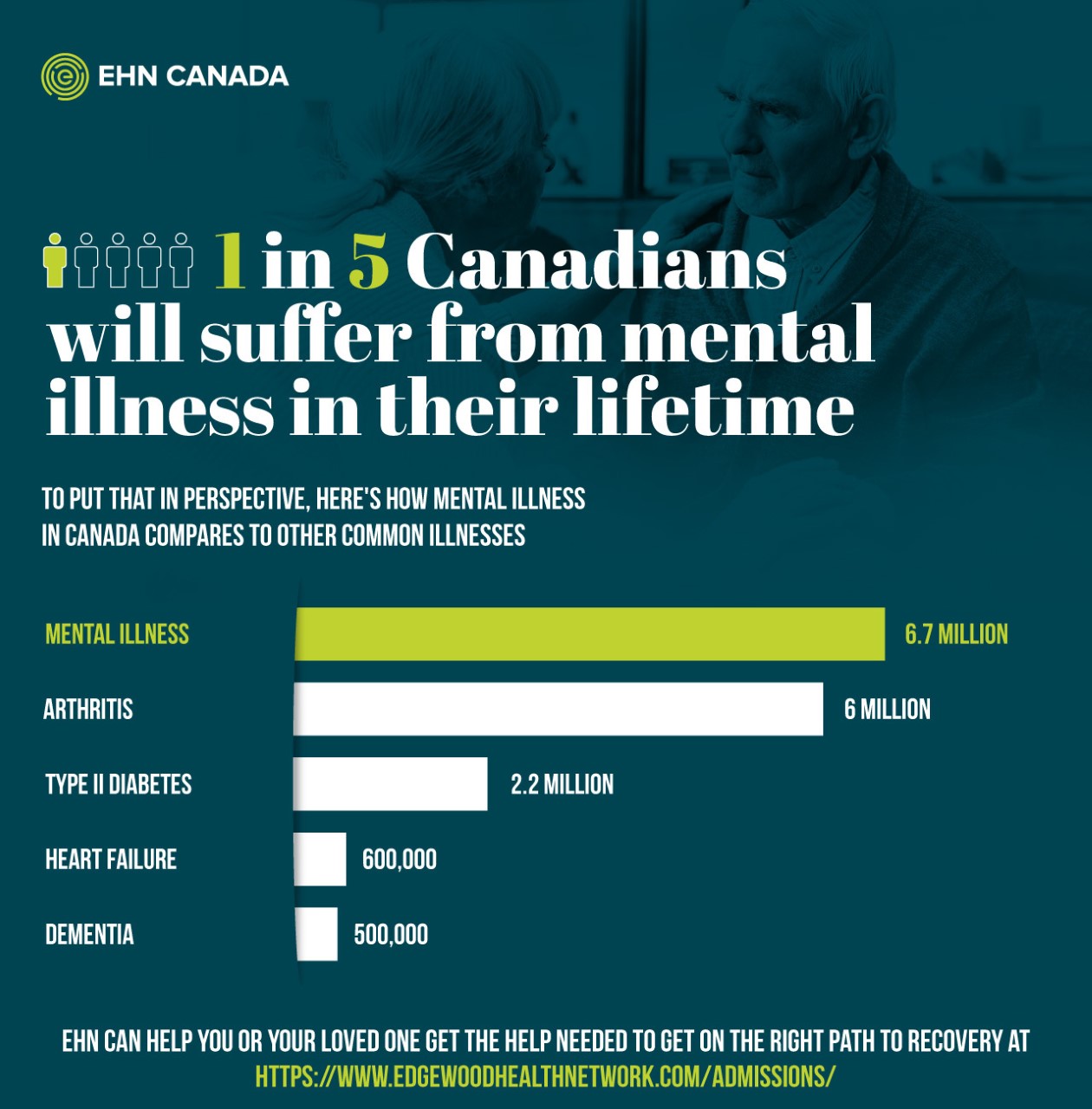
About 1 in 5 people will suffer from a mental illness during his or her lifetime. Today, we know that over 6.7 million people in Canada are coping with a mental illness. To put that in perspective, 2.2 million people in Canada have type 2 diabetes. [12] While the conversation around mental health becomes more inclusive, mental health disorders continue to affect more than most people think.
Signs you need to talk with a specialist
There’s a better chance of faster recovery if the problem is detected and treated at an early stage. Though it can be difficult to identify a concurrent disorder, there are a few indicators to look for:
Some signs of a mental health disorder:
- Mood swings, irritability and extreme changes in behaviour
- Not engaging/isolation
- Sleeping too little or too much
- Eating too little or too much
- Inability to manage stressful situations
- Feeling sad most of the time
Some signs of a substance abuse problem:
- No control over consumption
- Drinking to relax or to feel better
- Having blackouts and not recalling events
- Lying about your substance use
- Enjoying drinking more than being around people or doing a fun activity
- Deterioration of self-care
These are just some of the possible signs. Furthermore, signs manifest differently in every unique individual. A former patient shared 12 signs that helped her realize she had a substance abuse problem–find out here if her story sounds familiar.
If you relate to some of these signs or recognize them in a loved one, let our specialists help you. Our team is available 24 hours a day, 7 days a week. Talk with us in total confidentiality by calling 1 (416)-644-6345.
Ready to get help for a concurrent disorder? Here’s what to expect from treatment
Treating both disorders at the same time to achieve better results
Recognizing the signs of a mental health problem is crucial to long-term recovery. “Both major depression and alcohol dependence carry a significant risk for the development of the other”. [13]
As the Department of Psychiatry at Dartmouth Medical School confirms, “integrated treatment of both disorders has been shown to be more effective than separate treatments offered in parallel or in sequence”. [14]
When treating a concurrent disorder, the person has to get clean or sober first. Then there is a mental health assessment. The professional team can develop a treatment plan that addresses both the addiction and the mental health disorder. This treatment plan is called an integrated treatment, and has greater chances for success. Otherwise, “the dual nature of concurrent disorders can trigger a self-perpetuating cycle that contributes to poor outcomes, including a high risk of relapse if the disorders are not treated simultaneously”. [15]
So what does this mean? Imagine you have an addiction problem with a mental health disorder you don’t know about. You work hard for months and manage to get clean or sober. A couple of weeks later, a traumatic event happens to you (again). You run a significant risk of relapsing due to your mental health disorder being left untreated.
EHN Canada’s holistic approach
Our integrated treatments cover all the basics of health—the mind, body and soul. Through evidence-based treatment, you’ll learn to control your emotions, no matter what life throws at you. These skills will help you get better and stay better.
Here are evidence-based approaches to treatment for a co-occurring disorder:
- Dialectical behaviour therapy (DBT) is a skills-based treatment approach to teaching mindfulness, emotion regulation, distress tolerance and interpersonal effectiveness.
- Cognitive behavioral therapy (CBT) is an evidence-based treatment designed to help you have more positive thoughts, controlling the damaging negative ones.
- Group therapy is combined with individual therapy to provide ongoing support during and after treatment and has many benefits that facilitate rehabilitation. These sessions allow you to talk without being judged, to express your emotions and to meet people who experience similar problems.
A personalized treatment program is the most effective approach for a co-occurring disorder. Talk with one of our specialists to get the treatment you need.
Recovering from a co-occurring disorder
Post-treatment is the key to avoiding a relapse. You must continue the recovery process once you are discharged.
40% to 60% of in-patients who didn’t engage in post-treatment relapsed after 4 months.
COMPARED TO
83% of in-patients who joined at least one care/social group and had a successful outcome after 4 months.
We have many social groups and resources to support you after your treatment. You’re not alone. We can help you succeed. Here are just five of many reasons why aftercare is vital to sustainable recovery after you leave treatment.
Will I have this disorder all my life?
A concurrent disorder is a chronic biological disease, like diabetes. You will have it forever, but it can be effectively managed with treatment.
A person with diabetes cannot simply take one shot of insulin and go on with their life. A person who has a peanut allergy can never eat peanuts again, even if they stop for years. They need to find new recipes and restaurants to enjoy eating again without fear.
Someone with a co-occurring disorder can’t get healthy without changing their lifestyle. This doesn’t mean your life is over. You can be healthy and happy even if you are coping with a concurrent disorder. Part of the point of treatment and aftercare is to equip you with the tools and learnings to find new ways to thrive.
EHN Canada Can Help You
If you would like to learn more about the addiction and mental health treatment programs provided by EHN Canada, enroll yourself in one of our programs, or refer someone else, please call us at one of the numbers below. Our phone lines are open 24/7—so you can call us anytime.
References
[2] Quick Facts: Mental Illness & Addiction in Canada. Mood Disorders Society of Canada. https://mdsc.ca/docs/MDSC_Quick_Facts_4th_Edition_EN.pdf
[3] Gordon, Sherri, and Gans Steven. “Why Mental Health Disorders Co-Exist With Substance Use.” Addiction, Very WellMind, 16 January 2021, https://www.verywellmind.com/co-occurring-disorders-mental-health-and-addiction-4158280.
[4] Kuria, Mary, et al. “The Association between Alcohol Dependence and Depression before and after Treatment for Alcohol Dependence.” International Scholarly Research, Hindawi, 26 January 2012, https://www.hindawi.com/journals/isrn/2012/482802/.
[5] American Psychological Association. “Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults.” American Psychological Association, 24 February 2017, https://www.apa.org/ptsd-guideline/ptsd.pdf.
[6] CAMH. “CAMH Policy Advice.” Mental Health in Canada: Covid-19 and Beyond, CAMH, juillet 2020, https://www.camh.ca/-/media/files/pdfs—public-policy-submissions/covid-and-mh-policy-paper-pdf.pdf
[7] https://www.ccsa.ca/sites/default/files/2020-04/CCSA-NANOS-Alcohol-Consumption-During-COVID-19-Report-2020-en.pdf
[8] American Psychological Association qtd. by Bonanno, 2004, 59, 20-28. American Psychological Association. “Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults.” American Psychological Association, 24 February 2017, https://www.apa.org/ptsd-guideline/ptsd.pdf.
[9] American Psychological Association qtd. by Bonanno, 2004, 59, 20-28. American Psychological Association. “Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults.” American Psychological Association, 24 February 2017, https://www.apa.org/ptsd-guideline/ptsd.pdf.
[10] National Institute on Drug Abuse. “Common Comorbidities with Substance Use Disorders Research Report.” Common Comorbidities with Substance Use Disorders Research Report, April 2020.
[11] National Institute on Drug Abuse. “Common Comorbidities with Substance Use Disorders Research Report.” Common Comorbidities with Substance Use Disorders Research Report, April 2020.
[12] https://www.mentalhealthcommission.ca/sites/default/files/2016-06/Investing_in_Mental_Health_FINAL_Version_ENG.pdf
[13] Helen M. Pettinati, PhD , William D. Dundon, PhD. “Comorbid Depression and Alcohol Dependence.” Comorbid Depression and Alcohol Dependence, Psychiatric Times, 9 June 2011, https://www.psychiatrictimes.com/view/comorbid-depression-and-alcohol-dependence.
[14] F Brunette, Mary, and Kim T Mueser. “Psychosocial interventions for the long-term management of patients with severe mental illness and co-occurring substance use disorder.” Psychosocial interventions for the long-term management of patients with severe mental illness and co-occurring substance use disorder, National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/16961419/.
[15] Statistics Canada




