Your liver does a great deal for your body. It detoxifies many substances that could be harmful to you and makes new proteins, fats, sugars, and digestive enzymes among many other vital functions.i So, if anything compromises your liver health and it can’t do its job properly, you’re in serious trouble.
Understanding the Liver’s Role in Your Health
The liver is a vital organ that plays a central role in numerous bodily processes. From detoxifying potentially harmful substances to synthesizing essential proteins, fats, sugars, and digestive enzymes, producing proteins essential to health, the liver is truly a multifunctional powerhouse. A healthy liver is critical for removing toxins and waste from the bloodstream. When the liver is damaged and unable to function properly, toxins can accumulate and make you extremely vulnerable to disease or even death. Ensuring its health is crucial because if the liver becomes compromised and can’t function optimally, it can have serious repercussions for overall health. This is why understanding the liver’s role and ensuring its well-being should be a top priority for everyone.
Your Liver Needs Nutrition To Stay Healthy
Your liver needs nutrients just like all other organs in your body. Eating the right foods can support your liver in performing its functions. Certain nutrients are particularly good for liver health. But to understand why these nutrients have protective or healing properties, we must first understand what can go wrong with the liver.
Signs and Symptoms of Liver Damage
Early symptoms of liver damage often include fatigue, nausea, loss of appetite, jaundice (yellowing skin and eyes), and itching. Just as a scar might appear on the skin after a severe burn, fibrosis or scarring can occur in the liver when it experiences damage. This scarring can be the result of many factors, including excessive alcohol consumption or an overload of harmful substances, and indicates that the liver cells aren’t regenerating as they should. As liver disease progresses, more serious symptoms can develop like abdominal swelling, bruising easily, vomiting blood, and confusion or impaired brain function due to the buildup of toxins. Getting medical attention for suspected liver issues is crucial, as many liver diseases don’t show obvious signs until extensive damage has already occurred.
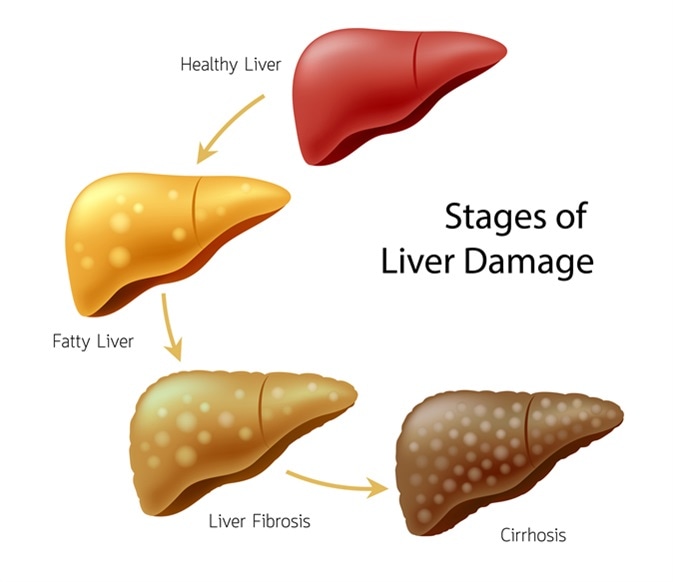
Stages of Liver Disease Progression
Liver disease doesn’t develop overnight. It progresses through various stages, starting with inflammation triggered by factors like excessive alcohol or toxins. This inflammation can lead to fatty liver disease, where fat accumulates within the liver. Left unchecked, this can advance to liver fibrosis, where the continued damage results in scarring. The most severe stages include cirrhosis, where liver cells die, and eventually, liver cancer. Catching liver disease early and making lifestyle changes can sometimes reverse damage before it progresses through these stages.
Which Foods Can Cause Liver Damage?
“Fibrosis” is a frequently-used term in relation to liver disease. Fibrosis is when tissue has thickened and scarred—usually in response to injury. When a tissue is damaged, it responds by trying to heal itself. The more severe the damage, the more a tissue will have to repair itself, and the more likely it is that scarring will occur.
For example, a severe burn on your hand is more likely to leave a scar after it heals than a slight surface scratch. It’s no different for the cells of your liver than for the skin cells on your hand. Tissue damage triggers healing, which can lead to fibrosis (scarring) when the cells aren’t able to fully form in exactly the same way as the original cells. Thus, anything that causes liver damage can lead to liver fibrosis.
Can any foods cause liver damage? One of the most damaging substances that many adults consume regularly is alcohol. When you drink alcohol—especially in excess—it damages the cells lining your liver and triggers inflammation.ii,iii Your liver cells respond in a way that results in fibrosis—they recruit even more inflammatory cells to the liver, which triggers the release of fibrogenic growth factors.3
Of course, many other drugs can cause liver damage. But liver damage and fibrosis caused by alcohol is so common that it has its own clinical diagnosis: alcoholic fatty liver disease (AFLD). This is when fats start to accumulate inside your liver as a result of excess alcohol consumption. AFLD can progress to more serious clinical conditions, including cirrhosis (liver cell death), liver cancer, and premature death.iv
What about foods that can cause liver damage? Dietary sugars, particularly refined sugars, found in desserts, soft drinks, sugary snacks, and confectionary are the biggest threat to your liver.v Fructose, a natural sugar found in honey and fruit, and high-fructose corn syrup (HFCS), a processed sugar that is added to many sweetened foods, increase risk of liver disease by encouraging fat to accumulate in the liver.5 They do this by:5
a) causing your body to produce its own fats, and
b) by impairing it’s ability to break down and eliminate fats.
What Is Fatty Liver Disease?
Fatty liver disease is the accumulation of fat inside the liver. It can lead to many long-term health complications if not effectively managed. The range of possible complications includes liver fibrosis (scarring), advanced fibrosis, liver cirrhosis (liver cell death), liver cancer, and even liver failure.vi,vii,viii
What happens if your liver fails? You’ll need to have a liver transplant, or you’ll die prematurely—yes, it’s scary! Your body can’t function properly without a healthy liver to effectively metabolize and remove toxins from your body. If you no longer have this critical defence mechanism in place, you become extremely vulnerable to disease and, possibly, death.
There are two types of fatty liver disease:
- AFLD is caused by excess alcohol consumption.
- Non-alcoholic fatty liver disease (NAFLD) is caused by factors other than excessive alcohol consumption.
NAFLD affects approximately 10–40% of adults worldwide because it’s strongly related to metabolic syndrome, which is very common.8 Syndromes are a group of symptoms that commonly occur together. The symptoms or clinical markers that are indicative of metabolic syndrome include the following:8
- Insulin resistance
- Diabetes
- Dyslipidemia (abnormal blood fat levels)
- Obesity
When NAFLD is left untreated, it can progress to non-alcoholic steatohepatitis (NASH), which is much more serious.5 “Steatohepatitis” means that the liver isn’t only fatty, it’s also inflamed. Inflammation is one of the factors that causes fibrosis by damaging liver cells. That’s why NASH is a very serious problem—the damage occurring to the liver is continuous and self-perpetuating.6,7,8
How Are Diet And Liver Health Related?
If NAFLD isn’t caused by alcohol, then what are its causes? Are any of them dietary?
As we discussed earlier, dietary sugars—especially refined sugars, fructose, and HFCS—pose the biggest threat to your liver.5 That’s why a high-sugar diet is so closely associated with the onset of NAFLD.5
Does this mean that by reducing your intake of sugary foods, you can help prevent NAFLD? Yes! Research suggests that if you consume less foods and drinks that are high in sugar, it may reduce fat accumulation in your liver, protecting you from NAFLD.5
How can you cut back on your overall sugar intake? Hidden or added sugars can creep into your diet in numerous ways. We’ve already mentioned fruit and honey. Many people disregard their sugar content because they’re natural and less processed. However, these foods are primary sources of fructose.
Another common category to watch out for is canned foods. Always be sure to check the sugars content on food labels to see how many grams of sugar a food contains per 100 grams (i.e., the percentage sugar). For example, if a serving size is 55 grams and there are 15 grams of sugar in each serving, that food is 27% sugar (15 divided by 55, multiplied by 100). That’s pretty high! Ideally, you want to choose foods that are less than 5–10% sugar to protect yourself against NAFLD.
How Sugars Impact Liver Health
Sugar, especially when consumed in excessive amounts, poses a significant threat to liver health. Refined sugars, fructose found in fruits and honey, and high-fructose corn syrup (HFCS) added to many foods can increase the risk of liver disease. They promote fat accumulation in the liver by boosting the body’s fat production and hampering its ability to break down and eliminate fats. By cutting down on foods and drinks high in sugar, one can significantly reduce the risk of developing fatty liver diseases and ensure a healthier liver.
Can You Improve Your Liver Health With The Right Diet?
Is there such a thing as nutrition for cirrhosis? Or a diet that’s ideal to prevent or reverse fibrosis before it progresses to cirrhosis?
Research suggests that dietary antioxidants, such as β-cryptoxanthin and astaxanthin, may be effective in preventing or treating NAFLD.6 This is because oxidative stress is a key factor in the development and progression of NAFLD.6 Oxidative stress happens all the time in human metabolism and is a natural part of the aging process. However, if your liver isn’t getting the antioxidants it needs to counterbalance it, oxidative stress can damage liver cells, leading to fibrosis and cirrhosis.6
Are there any other nutrients that can improve liver health? Research has shown that vitamin E therapy is effective at reducing steatosis (the amount of fat in the liver) and inflammation when given alongside pioglitazone (a type 2 diabetes medication).ix Vitamin E is actually used as a first-line pharmacological treatment for NASH because it’s a strong antioxidant.9 However, long-term use of vitamin E does have potential side effects, such as increasing the risk of prostate cancer and hemorrhagic stroke (a stroke caused by a ruptured blood vessel in the brain).9 Therefore, it’s best to consult with a qualified nutrition expert or naturopathic doctor before taking vitamin E to protect or heal your liver.
Diets rich in fibre and omega-3 fatty acids may also be good for the liver.x,xi Fibre is thought to have beneficial effects on gut flora (bacteria that lives in the gut) that reduce the amount of fats made within the liver.10,11 Omega-3 fats also appear to reduce fat production in the liver, as well as protecting the liver by reducing inflammation and helping to get rid of excess liver fat.10,11
Other nutrients that have been shown to heal or protect the liver include β-carotene, vitamin B12 (also called cobalamin), lycopene, and milk thistle extracts.6 Thiamine, also known as vitamin B1, is another essential nutrient that helps prevent against cirrhosis, specifically in AFLD.xii

Lifestyle Choices and Additional Support for Liver Health
Promoting liver health goes beyond just diet. Lifestyle choices play a crucial role in liver well-being. Minimizing the consumption of harmful substances, especially alcohol, can significantly reduce the risk of liver diseases. If one finds it challenging to control their alcohol intake, seeking help is vital. There are numerous support programs available for those struggling with alcohol consumption, ensuring they get the assistance they need to recover and maintain a healthy liver.
The most vital step is minimizing behaviors that directly damage the liver, especially limiting alcohol intake which can lead to AFLD. For support in controlling alcohol consumption, inpatient or outpatient treatment programs with counseling and group support can help overcome addiction. Maintaining a nutritious diet, active lifestyle, and healthy weight also enables the liver to function at its best.
Treatment Options for Liver Disease
The best approach to treating liver disease largely depends on its cause and severity. For conditions like alcoholic fatty liver disease (AFLD), reducing or eliminating alcohol consumption is paramount. For diseases caused by dietary factors, such as non-alcoholic fatty liver disease (NAFLD), dietary modifications, including reducing sugar intake, can be beneficial. In advanced stages, treatments may range from medications to manage symptoms, to liver transplants in the most severe cases.
29 Foods For Liver Health
As we just learned, the best foods to support liver health have one or more of the following properties:
- They protect against oxidative stress
- They reduce inflammation (directly or indirectly)
- They increase the breakdown of fats in the liver
- They reduce the production of fats in the liver
So, what are the top foods for liver health? Which foods contain abundant liver-protective or liver-healing nutrients?
The strongest antioxidants that can prevent NAFLD or stop it from progressing to NASH are found in vegetables, fruits, and pink-coloured seafood.6 The best anti-inflammatory foods also contain omega-3 fatty acids. Vitamins D and the B vitamins—specifically vitamins B1 (thiamine), B9 (folate), and B12 (cobalamin)—play a key role in supporting your liver health.10,12,xiii And anything you eat that feeds beneficial gut flora or encourages them to grow (namely, prebiotic and probiotic foods) will protect and support your liver.2
Based on this criteria, the following are the top 29 foods for liver health:
- Sweet red peppers – Red peppers contain antioxidants, such as β-cryptoxanthin and vitamin E, which have anti-inflammatory effects throughout the body.6,xiv
- Pumpkin – Pumpkin is another great source of β-cryptoxanthin, which prevents against oxidative stress in the liver.6,14
- Winter squash – Winter squash also contains β-cryptoxanthin, but keep in mind that prolonged cooking or processing can destroy this essential nutrient.6,14
- Persimmons – Persimmons are an excellent source of vitamin C, which is an antioxidant that improves liver fibrosis.10
- Tangerines – Tangerines are β-cryptoxanthin-rich, with the highest concentration of this antioxidant present during the ripening season.14
- Papayas – Papayas contain vitamin E, which is an antioxidant that plays a crucial role in reducing oxidative stress in the liver.10,14
- Salmon – Salmon contains an antioxidant called astaxanthin, which is even more effective than vitamin E in reducing liver inflammation and fibrosis.6
- Trout – Trout is a good source of vitamin B12, which is stored in the liver and associated with regulating fat throughout the body.6,13
- Lobster – Lobster contains vitamin B12 and astaxanthin. Did you know that astaxanthin gives lobster its red colour when cooked?6
- Shrimp – Astaxanthin, also found in shrimp, prevents against insulin resistance.6
- Tomatoes – Tomatoes, alongside other red fruits and vegetables, contain lycopene, which is an antioxidant within the family of plant pigments called carotenoids.6
- Red grapefruit – Lycopene is also found in red grapefruit and can reduce the risk of many cancers, including liver cancer.6
- Watermelon – Watermelon is a great source of lycopene, vitamin C, and vitamin A, which is a powerhouse of antioxidants!6
- Apricots – Apricots contain β-carotene, which gives apricots their orange colour and has protective effects on liver fibrosis, oxidative stress, and inflammation.6
- Liver – Liver is a great source of folate (vitamin B9), which has been shown to reduce liver damage caused by high-fat diets and excessive alcohol consumption.xv
- Kidneys – Kidneys are rich in vitamin B12. Did you know there is an association between low levels of vitamin B12 and metabolic syndrome?10,xvi
- Sardines – Sardines are a great source of omega-3 fatty acids, which protect against harmful fat build-up in the liver.10
- Clams – Clams are another high-quality source of omega-3 fatty acids and vitamin B12.10,16
- Beef – Beef contains vitamin B12, which helps prevent type 2 diabetes.6
- Tuna – Tuna is an oily fish that contains thiamine, which is often linked to excessive alcohol consumption.12,xvii
- Milk – Milk is an excellent source of vitamin D.xviii Interestingly, people with fatty liver disease commonly have low levels of vitamin D.10
- Eggs – Eggs contain omega-3 fatty acids, but only if you eat the yolk!10
- Chicory root – Chicory root is high in fibre, which has beneficial effects on your gut flora.10,xix
- Jerusalem artichoke – Jerusalem artichokes are another great source of fibre.19 Did you know that high-fibre diets can help prevent against fatty liver disease by helping to maintain a healthy body weight?19
- Onions (raw or cooked) – Onions contain flavonoids, which is another type of antioxidant that has positive effects on inflammation and oxidative stress.xx
- Bananas – Bananas are high in fibre.19 Studies show that people who don’t consume enough dietary fibre are more likely to develop liver disease.7
- Kefir (a fermented milk drink) – Kefir contains probiotics (live bacteria and yeasts), which contribute to healthy gut flora and digestion.7
- Kombucha (a fermented tea drink) – Kombucha is another drink containing probiotics.xxi By keeping your gut healthy, probiotics also reduce liver inflammation.7
- Yogurt containing bacterial cultures – Yogurt is another source of probiotics and thiamine, but remember to look out for yogurts high in sugar—too much sugar can actually cause your liver more harm than good!5,17,xxii
While eating these foods can help protect against liver disease, the best thing you can do for your liver is to minimize any direct, negative impact that your diet and lifestyle may be having on your liver.
If you’re having trouble controlling your alcohol intake, or if you or a loved one’s alcohol intake is starting to concern you, give us a call at 1-416-644-6345. We have both inpatient and outpatient support programs that can help you recover.
References:
1 Lala V, Minter DA. Liver Function Tests. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK482489/. Accessed March 8, 2020.
2 Albillos A, de Gottardi A, Rescigno M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J Hepatol. 2020;72(3):558-577. doi:10.1016/j.jhep.2019.10.003
3 Altamirano-Barrera A, Barranco-Fragoso B, Méndez-Sánchez N. Management strategies for liver fibrosis. Ann Hepatol. 2017;16(1):48-56. doi:10.5604/16652681.1226814
4 Younossi Z, Henry L. Contribution of Alcoholic and Nonalcoholic Fatty Liver Disease to the Burden of Liver-Related Morbidity and Mortality. Gastroenterology. 2016;150(8):1778-1785. doi:10.1053/j.gastro.2016.03.005
5 Jensen T, Abdelmalek MF, Sullivan S, et al. Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68(5):1063-1075. doi:10.1016/j.jhep.2018.01.019
6 Kitade H, Chen G, Ni Y, Ota T. Nonalcoholic Fatty Liver Disease and Insulin Resistance: New Insights and Potential New Treatments. Nutrients. 2017;9(4). doi:10.3390/nu9040387
7 Kolodziejczyk AA, Zheng D, Shibolet O, Elinav E. The role of the microbiome in NAFLD and NASH. EMBO Mol Med. 2019;11(2). doi:10.15252/emmm.201809302
8 Brunt EM, Wong VW-S, Nobili V, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primer. 2015;1:15080. doi:10.1038/nrdp.2015.80
9 Oseini AM, Sanyal AJ. Therapies in non-alcoholic steatohepatitis (NASH). Liver Int Off J Int Assoc Study Liver. 2017;37 Suppl 1:97-103. doi:10.1111/liv.13302
10 Suárez M, Boqué N, Del Bas JM, Mayneris-Perxachs J, Arola L, Caimari A. Mediterranean Diet and Multi-Ingredient-Based Interventions for the Management of Non-Alcoholic Fatty Liver Disease. Nutrients. 2017;9(10). doi:10.3390/nu9101052
11 Eslamparast T, Tandon P, Raman M. Dietary Composition Independent of Weight Loss in the Management of Non-Alcoholic Fatty Liver Disease. Nutrients. 2017;9(8). doi:10.3390/nu9080800
12 Bémeur C, Butterworth RF. Nutrition in the management of cirrhosis and its neurological complications. Journal of Clinical and Experimental Hepatology. 2014; 4 (2): 141-150.
13 Mahamid M, Mahroum N, Bragazzi NL, Shalaata K, Yavne Y, Adawi M, Amital H, Watad A. Folate and B12 levels correlate with histological severity in NASH patients. Nutrients. 2018; 10:440. doi:10.3390/nu10040440
14 Burri B, La Frano MR, Zhu C. Absorption, metabolism, and functions of β-cryptoxanthin. Nutrition Reviews. 2016; 74(2):69-82. doi: 10.1093/nutrit/nuv064
15 Xin F, Zhao Z, Zhang R, Pan Q, Gong Z, Sun C, Fan J. Folic acid attenuates high-fat diet-induced steatohepatitis via deacetylase SIRT1-dependent restoration of PPARα. World J Gastroenterol. 2020; 26(18):2203-2220. DOI: 10.3748/wjg.v26.i18.2203
16 Boachie J, Adaikalakoteswari A, Samavat J, Saravanan P. Low vitamin B12 and lipid metabolism: evidence from pre-clinical and clinical studies. Nutrients. 2020; 12, 1935. doi:10.3390/nu12071925.
17 Harvard T.H. Chan, School of Public Health. The Nutrition Source: Thiamin – Vitamin B1. 2022. Accessed on January 5, 2022 from: https://www.hsph.harvard.edu/nutritionsource/vitamin-b1/
18 Harvard T.H. Chan, School of Public Health. The Nutrition Source: Vitamin D. 2020. Accessed on December 14, 2021 from: https://www.hsph.harvard.edu/nutritionsource/vitamin-d/
19 Pérez-Montes de Oca A, Julián MT, Ramos A, Puig-Domingo M, Alonso N. Microbiota, Fiber, and NAFLD: Is there any connection? Nutrients. 2020; 12, 3100. doi:10.3390/nu12103100
20 Van De Wier B, Koek GH, Bast A, Haenen GRMM. The potential of flavonoids in the treatment of non-alcoholic fatty liver disease. Critical Reviews in Food Science and Nutrition. 2017; 57(4): 834-855.
21 Mayo Clinic. Consumer Health: What is kombucha tea? Does it have any health benefits? 2020. Accessed on December 14, 2021 from: https://www.mayoclinic.org/healthy-lifestyle/consumer-health/expert-answers/kombucha-tea/faq-20058126
21 Mayo Clinic. Consumer Health: What is kombucha tea? Does it have any health benefits? 2020. Accessed on December 14, 2021 from: https://www.mayoclinic.org/healthy-lifestyle/consumer-health/expert-answers/kombucha-tea/faq-20058126




